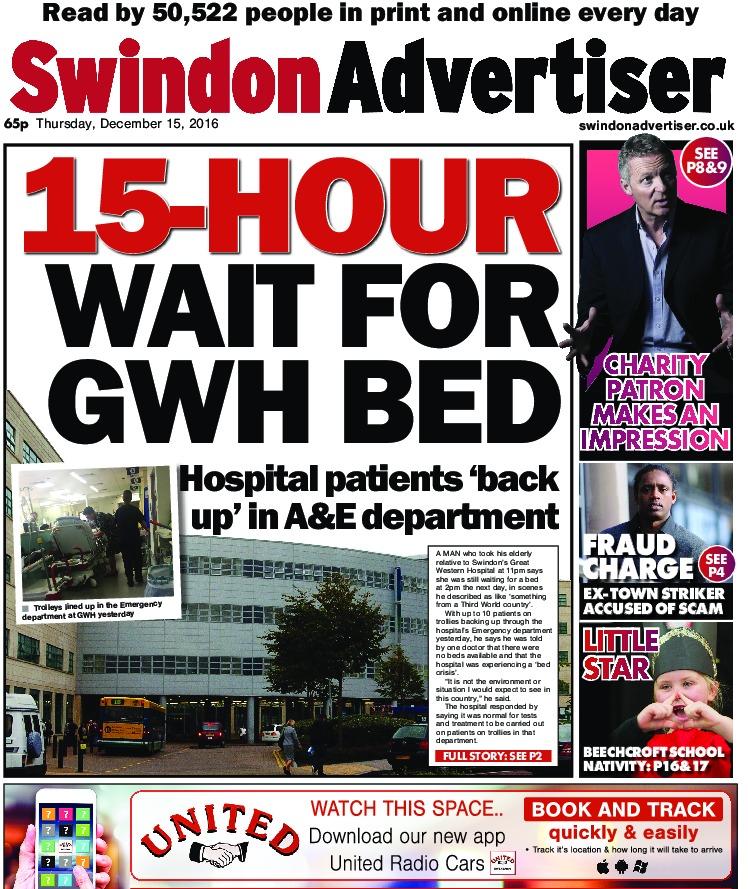
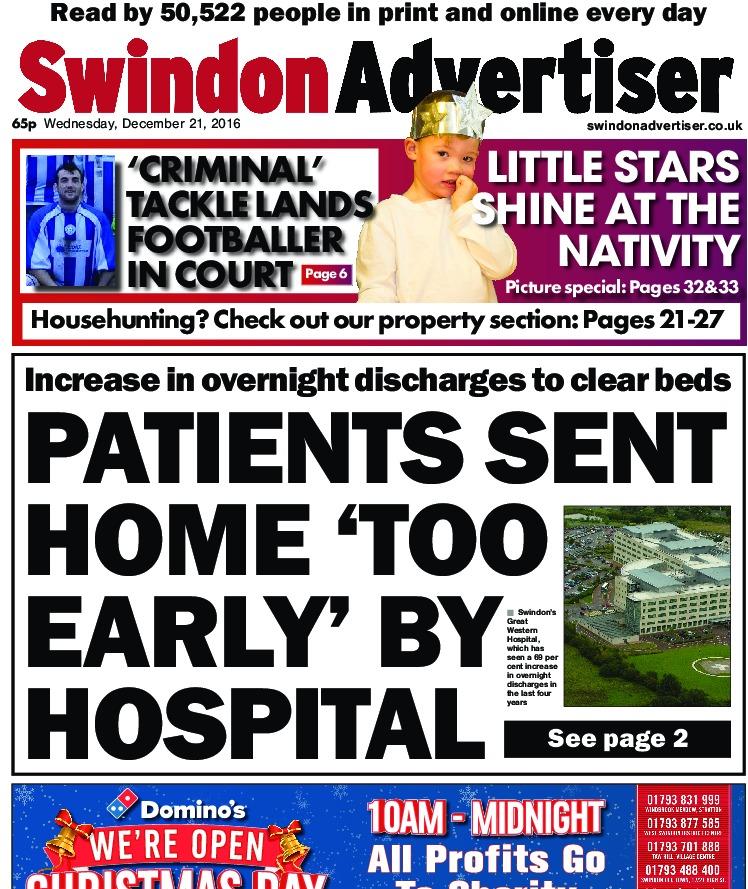
THE Great Western Hospital was at a state of red or black alert for at least 21 consecutive days last month.
Swindon’s only hospital is facing a perfect storm of long delays getting GP appointments, more people turning up at A&E and a social care crisis that is making it difficult to free up much-needed beds on the wards.
Hospitals measure the strain on their services using a four tier system, with level 1, or green, being the best case scenario and level 4, or black, indicating that organisations are unable to deliver comprehensive care.
Level 3, or red, is adopted when pressures are compromising patient flow and continuing to increase. It signals that urgent actions are required by partner agencies to alleviate the strain.
GWH spent two days on black alert and 19 on red between January 7 and 27 — information beyond this date is not yet available.
News of the continuing challenge being faced by the hospital comes as a report reveals that in November, the emergency department was only dealing with 71.8 per cent of patients within their four hour target.
The NHS says 95 per cent of patients should be seen in this time.
But responding to questions from councillors scrutinising the report, Gill May, executive nurse from the Swindon Clinical Commissioning Group, which arranges for the delivery of healthcare services in the town, suggested the figure was not helpful.
“Measuring the four hour target is missing the point, it’s a far bigger picture and that is purely a moment in time,” she said.
In terms of addressing the problem of movement of patients when they arrive at the hospital, Ms May said the CCG and the trust were “sinking in plans in terms of how we’re going to address this issue”.
But much of the problem exists beyond the grounds of GWH. On an average day the emergency department will see 225 people, of which 75 will need to be admitted.
Doctors are reminding patients that A&E is for life-threatening emergencies and not issues like toothache, coughs and colds or even broken fingernails.
But the numbers coming through the doors may not be the issue.
Ms May told councillors that on any given day, 80 people were fit to leave the hospital, meaning there should be excess space available and not a bed deficit.
But deficiencies in community care — in people’s homes as well as in residential facilities — means the hospital is bearing the brunt of the pressure and is unable to share the burden across the sector.
Ms May added: “We simply have to provide more care in the community setting and that is something we need to look at.”
Following the closure of SEQOL, the GWH Trust took over more community health services and the hope is that this change will allow them to introduce greater coordination.




Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel