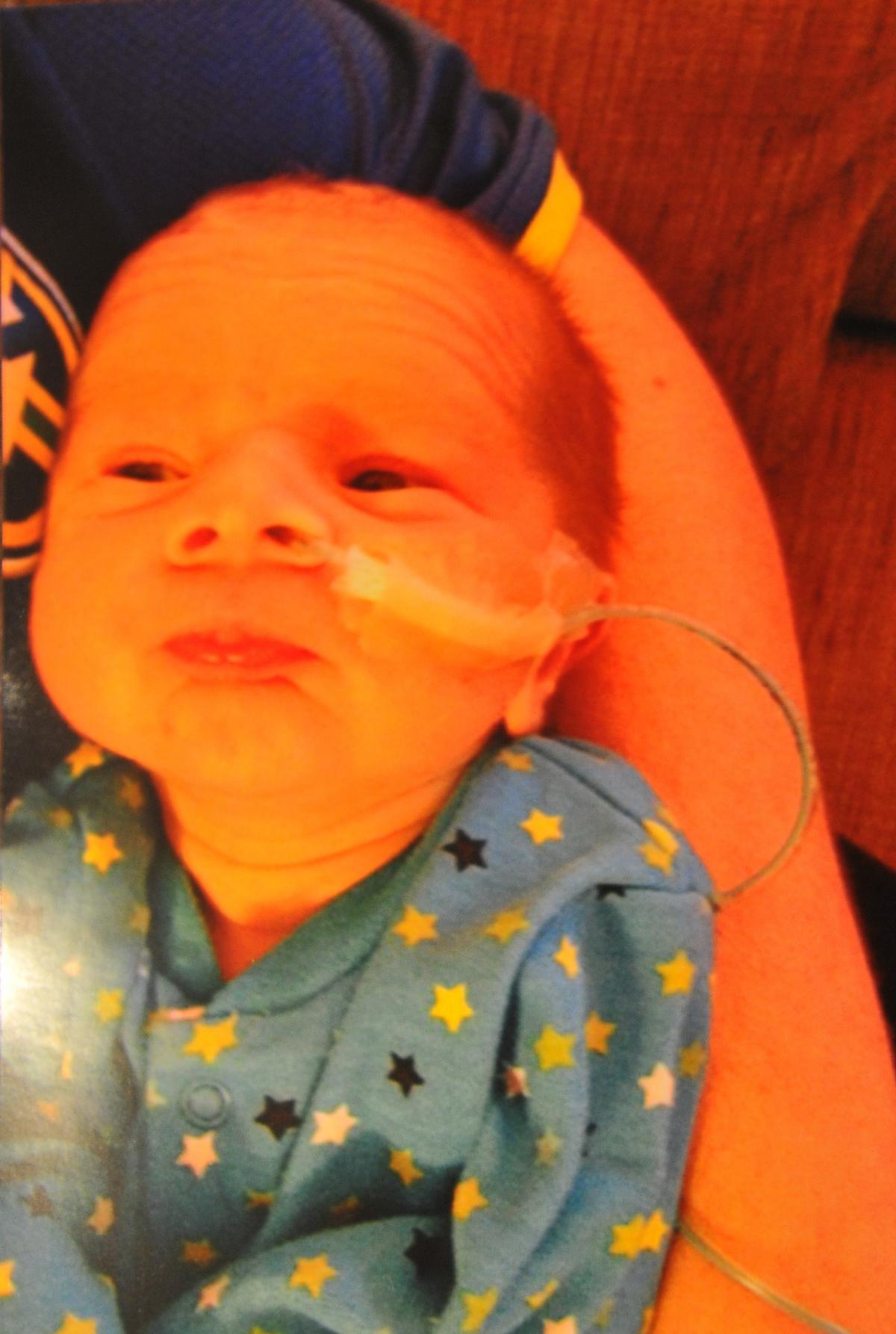
THREE years after his passing at just 17 days, Jo and Mark Fry remember their son Charlie and pay tribute to Helen House, the hospice where they shared precious moments with him.
THAT final day with him three years ago, the family took it in turns to hold and cuddle Charlie, committing to memory his scent, soft features and the furrow of his brow in the warmth of his hospice room.
As the 17-day-old infant was returned to his mother, he slipped away wrapped in her arms.
“Mark’s dad had read a story to Charlie and we were all in the room together. He was being passed around to have cuddles. When he was passed back to me he slipped away. It was all very peaceful,” says Jo with emotion.
“I was relieved that he wasn’t in pain anymore but devastated to have lost him.”
Jo’s pregnancy had passed seamlessly, until her 20-week scan at the Great Western Hospital revealed complications with the foetus’s bowel.
Unsure what the issue might be, Jo was referred to John Radcliffe Hospital in Oxford for further tests where consultants picked up a blockage in his gut. This meant the amniotic fluid was unable to pass through his body, instead building up around him.
Although concerned doctors were not alarmed. Jo and Mark were reassured that surgery after the birth would allow their baby to recover.
Charlie was born on May 6, 2012. It is not until two days later, during the procedure that surgeons realised the full extent of his ailment.
He was diagnosed with short gun syndrome, a condition in which the bowel is shorter than normal. In Charlie’s case the bowel had grown into a series of miniature sections all blocked off from one another preventing him from absorbing any fluid, vitamins and other nutrients needed to survive.
Only a transplant could potentially save him – and this could not happen until he reached the age of four.
Even then his chance of survival would remain minimal.
“They were very honest with us,” recalls Jo. “They advised that not doing anything at this point was the best thing to do. They explained his bowel looked like little sausages joined together – there was no hole for anything to pass through him.
“ There would be a potential for a transplant when he was four years old but in that time his quality would have been very poor. He would have to live on TPN, total parenteral nutrition, to feed him through a long line and get nutrition in his system. They had already tried to get a long line in his vein but couldn’t get it in. Even if we tried to go down that route the chance of survival would not be good.”
Then and there Jo and Mark decided to let their son go and spare him years of agonising pain.
“We didn’t want him to suffer and yet you want to keep hold of your child,” says Mark, an employee at Crown Timber in Cirencester.
“The next day we told doctors we wanted to let him go naturally.”
Unsure about the future, they however were certain of one thing - their son would no spend his remaining days in hospital. A nurse suggested they contact Helen House, a children’s hospice in Oxford.
When a room became available at the hospice that week, the family moved in. Charlie was five days old.
“Charlie had his own room in Helen House where the staff would look after him but Jo and I decided to keep him with us in the accommodation Helen House provided, to make the most of our time together,” continues Mark, 43.
“The staff would pop in to check on Charlie and were always around if we needed help or a bit of time to ourselves. They fed us three meals a day, did our laundry. Nothing was ever too much trouble. They let us get on with our lives and focus on Charlie.”
Unable to feed their child, they watched powerless as he whimpered with discomfort in the night. He was placed on morphine and the dosage gradually increased to allow him to bear the pain.
Over the 12 days they spent with Charlie at the hospice, the family only left Oxford once, to bring their newborn home for the first and last time.
“We had set up his room for him and we wanted him to at least see his home once,” smiles Jo.
The journey to Swindon was nerve-wracking in many ways.
“I felt like I was driving a precious cargo,” remembers Mark. “I don’t think I’ve ever driven so slowly. Going home was right, we felt he should see the things we had done to make it his home.”
From reading bedtime stories to bathing their child or taking him out for walks, on their return to the hospice they endeavoured to lead a life as normal as possible under the circumstances.
“We just took it day by day and tried to appreciate everything,” says Mark. “We took so many pictures. You don’t know when the last picture is going to be. You could see him getting thinner and thinner.
“I remember giving him his first bath. It’s something you take for granted but he had wires coming in and out of him and it was a tricky situation. But the staff got the baby bath and helped us bathe him. It was special for me.
“One of the lasting memories for me was being in the sensory room and I lay down on a mat and I fell asleep with my son on my chest.”
Jo cherishes the hours Mark spent reading Thomas the Tank engine to their son.
“We tried to build memories with Charlie,” she says. “We never had any idea how long we might have with him. One of the thing that always touched me is when Mark read him bedtime stories at night. Charlie was always quite settled during the stories.”
By the time Charlie passed away on May 23, he had grown thin and due to the lack of fluid, unable to close his eyes or blink.
“We thought he had gone in the night, the day before,” adds Jo. “His breathing had got very heavy the night but he was still with us. The last 24 hours I had found myself checking he was still breathing.
“I don’t know that you ever move on. Even now; three years on there are days when you just break down.”
Mark adds: “When he passed away I was happy he would not have to suffer any more pain. But you feel empty. There is so much more you wanted to do but never got to. It all happened so quickly.”
18 months after Charlie’s passing, the couple welcomed their second child, Joseph.
Since 2012, they have kept Charlie’s memory alive by collecting funds for Helen House and its young adult hospice Douglas House.
For the second year, Mark will join the Rainbow Run in Reading on June 21. So far he has received £155 in donations.
“For those 12 days we feel as though that was a family and we were part of it,” says Mark. “They couldn’t have done anything more to help us. Whatever we needed, no matter how big or small or the time of day they would have got it for us. That’s on top of the care they gave Charlie. They allowed us to make the most of our time with him.”
To sponsor Mark go to https://secure.helenanddouglas.org.uk/registrant/FundraisingPage.aspx?registrationID=472953&langPref=en-CA#&panel1-2
To make a donation to Helen & Douglas House got to www.helenanddouglas.org.uk.
PANEL 1
• Short bowel syndrome, also referred to as SBS, or short gut syndrome, is a disorder in which a significant amount of bowel (half or more of the small intestine) is lost, removed, or unable to function inside the body.
• In severe cases feeding may have to take the form of fluids given into a vein (usually via a long line). Over the next weeks or months the baby's intestine becomes able to absorb special milk and can be discharged home. Eventually the baby may be able to tolerate normal milk and food.
• In extreme cases there is not enough intestine present for the baby to survive without TPN for many months or even years. Unfortunately many of these babies die often after months or years in hospital due to complications of TPN treatment. However bowel transplant operations are available and are becoming more successful.
• In newborn infants, the 4-year survival rate on parenteral nutrition is approximately 70 per cent. In newborn infants with less than 10 per cent of expected intestinal length, 5 year survival is approximately 20 per cent.
PANEL 2
• Helen House in Oxford was the world's first children's hospice when it opened its doors in November 1982.
• It sprang from the friendship between Sister Frances Dominica and the parents of a seriously ill little girl called Helen who lived at home with her family but required 24 hour care.
• The hospice provides medical, emotional and practical support, helping families deal with the implications of living with a child who will die prematurely, so they can make the most of their time together.
• The hospice launched Douglas House in February 2004 specifically designed for young adults aged 16 to 35. The hospices are now known as Helen & Douglas House.
• It costs £5m a year to run both hospice houses. 85 per cent of the sum comes from donations.








Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel